What is a CVA (Stroke)?
A Cerebrovascular Accident (CVA), commonly known as a stroke, happens when the blood supply to a part of the brain is disrupted. This interruption prevents brain cells from receiving the oxygen and nutrients they need, leading to cell death and potentially long-lasting neurological damage.
Strokes can cause a wide range of physical, cognitive, and emotional challenges, depending on the area of the brain affected. Early diagnosis and immediate medical attention are critical, but so is the rehabilitation process, which plays a major role in recovery and improving quality of life.
Type of Stroke
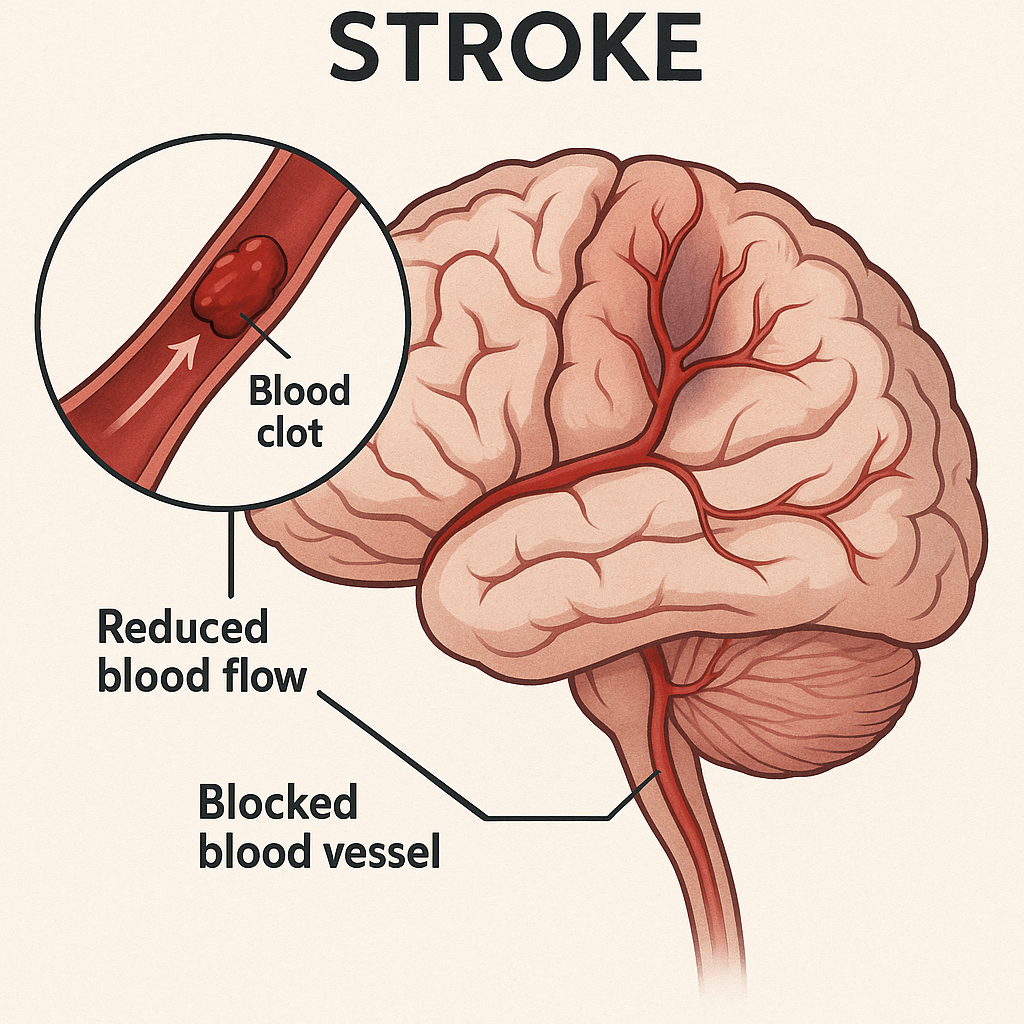
1.Ischemic Stroke (≈85% of cases)
- Caused by a blocked artery, usually due to a blood clot or narrowing of the vessels.
- Common subtypes include:
- - Thrombotic stroke (blood clot forms in the brain)
- - Embolic stroke (clot forms elsewhere and travels to the brain)
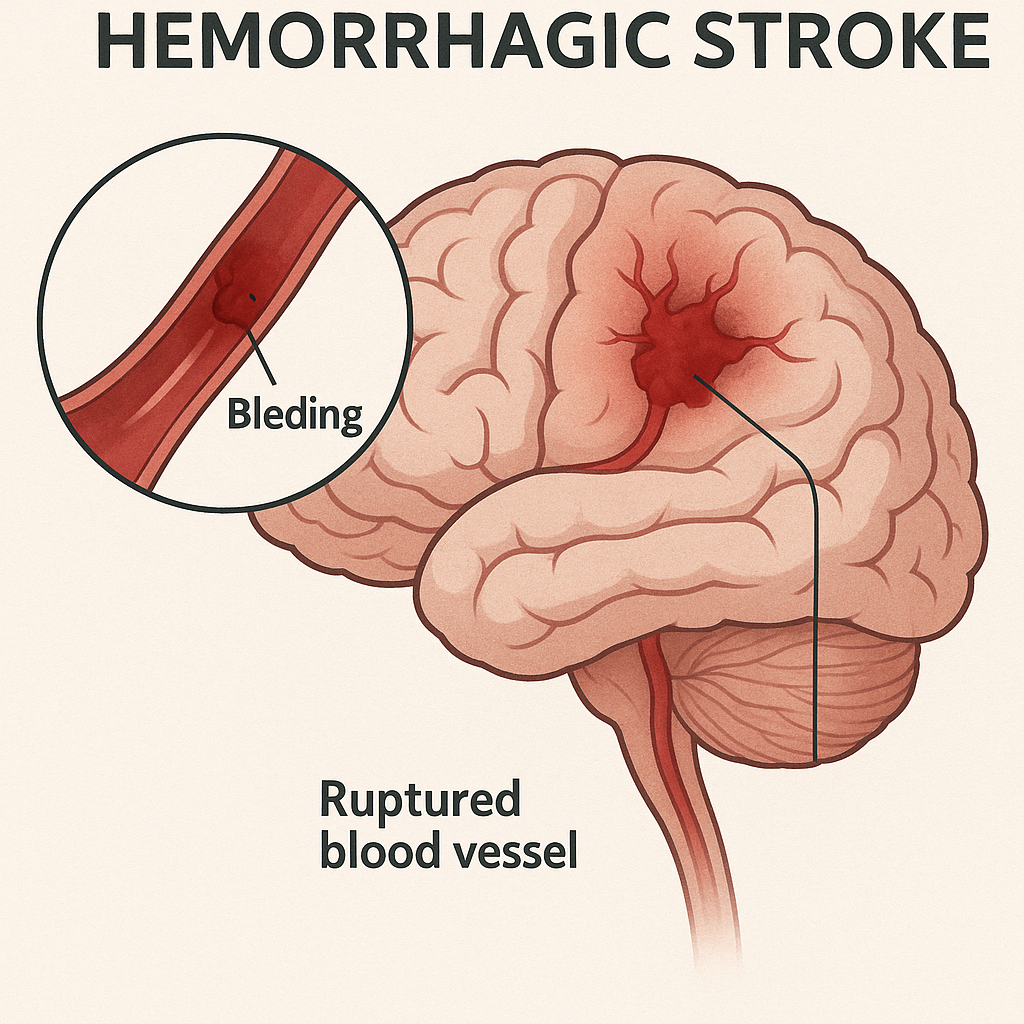
2.Hemorrhagic Stroke (account for 13-28% of all strokes and carry a 10-15% risk of death)
- Caused by a ruptured blood vessel, leading to bleeding in or around the brain. Often associated with high blood pressure or aneurysms.
3.Transient Ischemic Attack (TIA) - “Mini Stroke”
- A temporary blockage that resolves within 24 hours, but it’s a serious warning sign of future strokes.
Symptoms of a Stroke
Recognizing the signs of a stroke early is crucial for immediate medical intervention. Stroke symptoms can appear suddenly and may include:
- Sudden numbness or weakness – Particularly on one side of the body, affecting the face, arm, or leg.
- Confusion or trouble speaking – Difficulty understanding speech, slurred speech, or trouble finding words.
- Trouble seeing – Sudden loss of vision or blurry vision in one or both eyes.
- Difficulty walking – Dizziness, loss of balance, or coordination problems.
- Severe headache – A sudden, severe headache with no known cause, often accompanied by nausea or vomiting.
- Sudden trouble swallowing – Difficulty swallowing or feeling as if food or liquid is stuck in the throat.
F.A.S.T. – A Quick Way to Recognize Stroke Symptoms
- Face: Ask the person to smile. Does one side of their face droop?
- Arms: Ask the person to raise both arms. Does one arm drift downward?
- Speech: Ask the person to repeat a simple sentence. Is their speech slurred or strange?
- Time: If you observe any of these signs, it’s time to call emergency services immediately.
Risk Factors
- High blood pressure (most significant risk)
- Diabetes
- Heart disease
- Smoking and excessive alcohol
- Sedentary lifestyle
- Obesity
- High cholesterol
- Family history of stroke
- Previous stroke or TIA
- and others
Role of Physiotherapy
Physiotherapy plays a critical role in the rehabilitation of individuals who have experienced stroke. The goal is to help the patient regain as much function and independence as possible and to prevent complications.
In stroke (CVA) rehabilitation, physiotherapists use several approaches or treatment concepts depending on the patient’s needs, recovery stage, and impairments. Here are the main physiotherapy approaches commonly used:
1. Neurodevelopmental Treatment (NDT) / Bobath Approach
- Focuses on normalizing muscle tone and facilitating normal movement patterns
- Involves handling techniques to guide and assist movement
- Emphasizes postural control, balance, and functional activities
- Aims to inhibit abnormal reflexes and synergies
- Widely used and adaptable to different stages of recovery
2. Brunnstrom Approach
- Based on using synergistic movement patterns (common after stroke) to initiate voluntary movement
- Progresses through stages of motor recovery
- Encourages reflex activity early, then transitions to voluntary control
- Useful in early stages when spasticity and synergies are present
3. Proprioceptive Neuromuscular Facilitation (PNF)
- Uses diagonal movement patterns and sensory cues (e.g., stretch, pressure) to improve motor control
- Enhances strength, flexibility, and coordination
- Can be used to facilitate both upper and lower limb function
4. Mirror Therapy
- Involves performing movements with the unaffected limb while watching its reflection in a mirror placed between the limbs
- Creates the illusion that the affected limb is moving normally
- Helps with motor recovery and reducing neglect or pain
💡 Especially helpful for upper limb recovery
5. Task-Oriented Training / Functional Training
- Involves practicing real-life tasks (e.g., standing up, walking, reaching, climbing stairs)
- Encourages problem-solving and motor learning through repetition
- Focuses on independence and function
- Useful at all stages and tailored to patient goals
6. Motor Relearning Program (MRP)
- Encourages active participation in learning motor tasks
- Focuses on analyzing and correcting movement patterns
- Emphasizes practice in varied environments
7. Balance and Vestibular Training
- For improving postural control, reducing fall risk, and enhancing spatial orientation
- Includes exercises like weight shifting, standing on unstable surfaces, and gaze stabilization
Why Physiotherapy is Important and the Need to Start Early ?
The first six months after a stroke are often considered a "golden window" for recovery, as this period offers the greatest potential for neuroplasticity—the brain's ability to reorganize and form new neural connections. Engaging in physiotherapy during this time can significantly enhance recovery outcomes, helping individuals regain movement, strength, and independence.
Starting physiotherapy as soon as possible accelerates recovery by engaging the body in rehabilitation while the brain is still highly receptive to change. The early intervention period maximizes the effects of rehabilitation, leading to better long-term outcomes.
Remember, while the first six months are crucial, recovery doesn’t stop there. Ongoing physiotherapy, even beyond this period, continues to enhance recovery and can help maintain or improve functional abilities over time.